Vitrectomy
Vitrectomy is a surgical procedure used to treat problems of the eye’s retina and vitreous. The vitreous is a clear jelly-like substance which occupies about two-thirds of the eye.
Vitrectomy is a surgical procedure used to treat problems of the eye’s retina and vitreous. The vitreous is a clear jelly-like substance which occupies about two-thirds of the eye.
It lies behind the iris (the coloured part of the eye) and the lens, and in front of the retina (back of the eye).
Composed of over 99% water, the vitreous also contains collagen fibres, proteins and a viscous substance – hyaluronan.
It has no real function other than providing volume to the eye.
Vitrectomy is a surgical procedure to remove the vitreous.
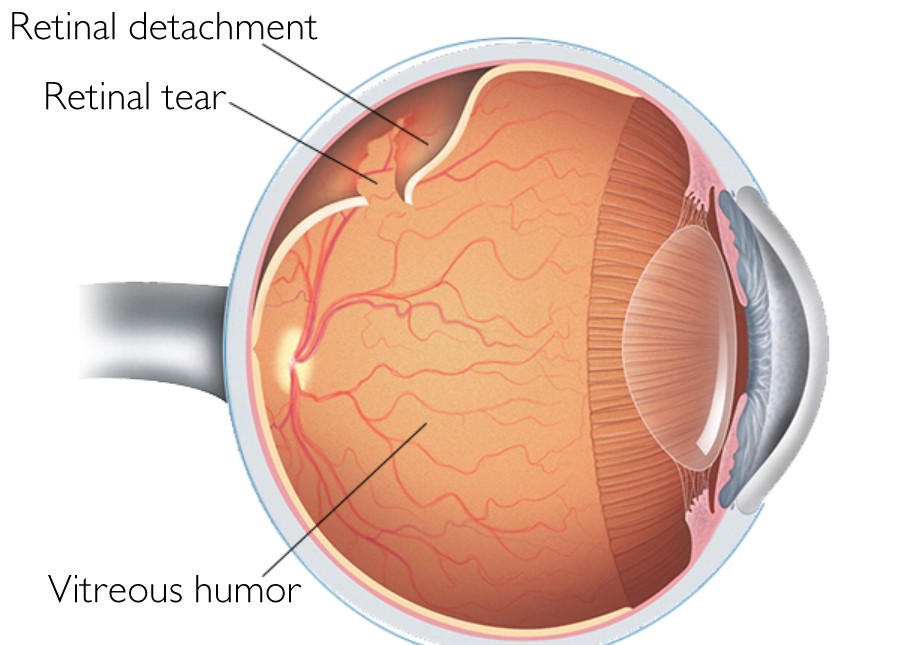
Vitrectomy is often part of another eye treatment e.g. when surgical repair is required for the retina when is detached. Your consultant ophthalmologist may recommend a vitrectomy if you have one of these conditions:
Following a detailed assessment, your Consultant Ophthalmic Surgeon will discuss the best course of treatment for you. The consultant will be the same person who carries out your procedure and your checks at follow-up appointments.The consultation process is very detailed and can take up to 3 hours. Tests and investigations are performed by nurses, optometrists and technicians. You will be provided further information about the procedure and shown video animations.
You will then be seen by an experienced fellowship-trained consultant who will evaluate your eyes and come to a final decision. The consultant will inform you about what options there are for your eye and explain the process further with expectation of outcomes following surgery. You will be provided with an informed consent.
A vitrectomy is performed in an operating theatre using either a local anaesthetic. Three tiny openings are made in the sclera and delicate instruments are inserted into the eye. Vitreous cutters, forceps and scissors remove the vitreous gel and scar tissue that may be growing on the surface of the retina. A fibreoptic illuminator is used to light the inside of the eye during the operation.The vitreous gel is replaced by either saline solution, air, or gas, all of which are replaced by the eye’s own fluid over time. The vitreous does not grow back and the eye is able to function well without it. Sometimes, silicone oil or heavy liquid is inserted into the vitreous cavity at the end of the procedure and this will require another operation for its removal at a later date. Occasionally, a silicone band is encircled around the eyeball to assist with reattachment of the retina.
Your consultant ophthalmologist will prescribe medicine to help relieve pain. You will also be given eye drops to use for up to 4 weeks. Visual recovery after surgery varies greatly from patient to patient, depending on the underlying condition for requiring a vitrectomy in the first place and the type of substance inserted into the vitreous cavity at the end of the surgery.If gas or oil has been inserted into the vitreous chamber you may be advised to position your head tilted downwards. This helps to make sure that the gas or oil is lying against the area of the retina which has been treated. Your surgeon will specify the duration required. You will not be able to fly for 6 weeks if you have gas in your eye.Your follow-up appointments are usually booked within 1-2 weeks after surgery. It is common after vitrectomy for a cataract (clouding of the lens) to develop. At some stage you are therefore likely to need cataract surgery. The possibility and timing of this secondary surgery will be discussed before vitrectomy treatment.
Severe complications are rare and anatomic success for vitrectomy is over 90% for many conditions. Advances in instrumentation, techniques, and understanding of diseases of the vitreous and retina have made vitrectomy and retina surgery more successful.Surgery for diseases that were once incurable, such as macular hole, is now routinely performed with excellent results. The list of indications for vitreous surgery continues to grow. The ability to directly work on or near the retina holds great promise for the future, not only to prevent vision loss, but to restore and enhance our ability to see.
There is a 5-10% risk of needing further retinal surgery after vitrectomy. The risk of developing a cataract is approximately 30-40%.
Upon insertion, the gas bubble rises and applies pressure to the area that needs healing. However, since the retina is at the back of the eye, and the gas bubble rises, in order to apply pressure on the retina, the head needs to be positioned downwards.
You will need 2 to 4 weeks to recover before you can do your normal activities again. It may take longer for your vision to get back to normal. You might have some pain in your eye for a few days after the surgery.
Gas bubbles placed in the eye during vitrectomy surgery can last from 1 week to 8 weeks depending on the gas used. The gas will resolve spontaneously. It is important that you continue to follow up with your surgeon.
[surgeonsv]
I understand that all my data, clinical and otherwise will be protected under GDPR. I understand my data may used for the purposes of quality improvement and advancement of eye care such as audit. This is a component of good clinical governance and measures will be taken to ensure my data is not identifiable.