Side Effects
Laser eye surgery is revolutionary and life-changing for patients. Like all surgical procedures there are risks involved that can be minimised or eliminated. The most important way to minimise risk is to seek out a good surgeon that you can trust with a known track record. It is important that the operating surgeon or one who is equally able to perform the surgery personally examines you at consultation. Additionally the operating Centre must have all the necessary diagnostic technology, as well as care pathways and trained staff to ensure all testing performed is complete and to a high standard.
You MUST educate yourself well and here are some of the specific risks reported and how they can be minimised or eliminated.
1. Dry eye
Dry eye following laser eye surgery is typically a temporary phenomenon but can become a longer term problem if patients are not evaluated properly before surgery.
Dry eye following LASIK and PRK occurs because the superficial nerve endings on the surface of the cornea need to regenerate and heal. The cornea is a little numb and does not have the sensation required to trigger tear production. Additionally nerve endings are known to produce chemical messengers (cytokines) which act as growth factors coordinating interaction between surface cells. Nerves regenerate in 6 to 12 weeks and during this time the eyes are prone to getting dry.
Long term dryness can occur if there is an underlying problem that has not been diagnosed and treated adequately before surgery.
Symptoms: Grittiness, burning, fluctuating vision, pain
Avoidance:
- Make sure the operating centre performs dry eye tests including a – a) Schirmer’s test for tear production and b) Tear Break-Up Time (TBUT). Make sure your operating surgeon is also experienced and knowledgeable about dry eye.
- Ask your surgeon if you have Meibomian Gland Disease. Meibomian glands are located in the eyelids and produce vital oils which helps to prevent tears from evaporating too quickly.
- In advance of your laser eye surgery, consider taking re-esterified Omega 3 supplements to improve your Meibomian gland function.
- Take preservative free eye drops frequently after your procedure
- Take breaks from computer monitors every 20 mins, close your eyes for 20 seconds and look out of the window for 20 seconds – then get back to work.
2. Halos and Glare
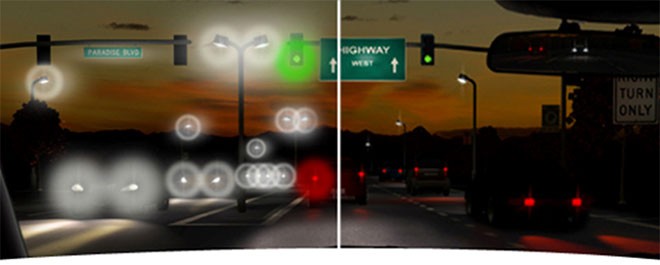
For a few days to a few weeks following Laser eye surgery (both Lasik and surface ablation), ALL patients experience halos. This is because fluid within the recently treated cornea causes light to scatter. Once the fluid clears, the halos disappear. Some patients however develop permanent halos following surgery and find their symptoms is worse at night (left hand image). This problem is caused by induced aberrations from lasers which have delivered small diameter zones of correction or older forms of treatments that are not Aspheric in profile. The good news is this problem does not occur very often as long as patients are selected correctly and the correct treatment customised for each eye is delivered correctly. This problem can also occur if the treatment has not been centred correctly.
Avoidance:
- Ensure your pupil size is measured in dim/dark light
- Ensure your surgeon is experienced in Laser eye surgery and understands the significance of high order aberrations.
- Ask your surgeon if you will be receiving an ASPHERIC treatment profile on your cornea. Good cameras and spectacles have “Aspheric” lenses to provide good quality vision. You want to be sure your surgeon plans on making your cornea aspheric.
- Ensure the treating centre has laser technology that is up to date and well maintained.
3. Infection
Like all surgical procedures, there is a risk of infection. Fortunately the risk of infection in laser eye surgery is extremely small. The risk of infection from highest to lowest is LASEK, PRK, blade -LASIK and IntraLASIK with a femtosecond Laser carrying the lowest risk of all. The overall risk of infection after intraLASIK in very good eye centres is 1 in 10,000 cases.
Avoidance:
- Go to a reputable centre which has an excellent Care Quality Commission (CQC) rating
- Ask about the environment in which laser eye surgery is being carried out. Is the air HEPA filtered and what is the exchange rate per hour ? 10 per hour is the minimum required, many use 15 per hour.
- Ask what antibiotics are used in preoperative preparation and during surgery. Ideally a 4th generation fluoroquinolone such as Moxifloxacin or Gatifloxacin. These antibiotics are very strong and eliminate a wide variety of bacteria.
4. Ectasia
This is a condition where the cornea is more elastic than usual and following laser eye surgery can become unstable. The cornea becomes “ectatic” in other words bulges and thins over time. This results in a change in vision with the requirement to initially wear glasses. Astigmatism increases and causes continuing problems. Ectasia can occur in both Lasik and PRK/LASEK surgery. There are tell-tale signs on the cornea that can be picked up using sophisticated corneal mapping, biomechanic checks and corneal epithelial thickness mapping
Avoidance:
- The best person to be able to determine whether you are at risk or not is a surgeon who has specialised in the Cornea. Specialised corneal surgeons are trained and experienced with Keratoconus, a condition where the cornea is elastic and bulges. They are very familiar with the type of tests used to check for this condition as well as subtle signs of the condition.
- Ask if 3 dimensional tomography devices like the Pentacam is being used to evaluate the cornea
- Does the centre use biomechanical checks to determine corneal elasticity
5. Flap complications
Flap complications such as buttonholes, partial flaps, irregular fragmented flaps have been reported in Lasik laser eye surgery where a blade microkeratome is used to create the flap.
Following the introduction of the IntraLASE femtosecond laser for flap creation (introduced to UK by Centre for Sight in 2004), flap complications are now thankfully rare. Use of the femtosecond laser is the gold standard and blade microkeratomes that in the past were responsible for flap complications should no longer be used.
Avoidance:
- Ask the treating centre if the IntraLASE laser will be used for creating the corneal flap in the LASIK procedure
- Ask your surgeon how long they have performed LASIK and for how long they have used IntraLASE.
Laser eye surgery is a fantastic procedure that is liberating. It is important that you make a good choice. Becoming well educated is a good first start. Next find a good surgeon and eye centre who can deliver phenomenal care. A good tip is go where other eye surgeons go for their own care.
Author Information
Authored by Sheraz Daya MD FACP FACS FRCS(Ed) FRCOphth, Consultant Ophthalmic Surgeon & Medical Director, June 2019.
