Your Guide to Laser Lens Replacement
At Centre for Sight, a laser (rather than a manual technique) is used to assist the process in Lens Replacement / Exchange and is performed in this manner in 100% of cases and at no additional cost. Learn more about the treatment.

What is Lens Replacement Surgery?
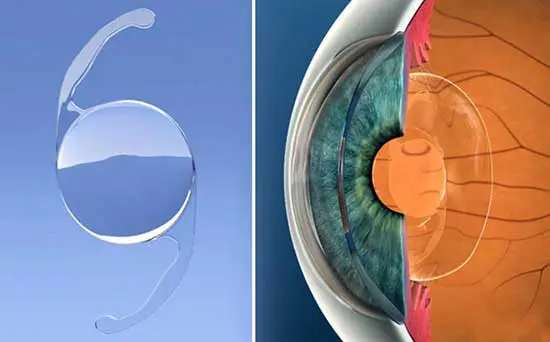
Behind the pupil in the eye is a lens that is used for fine focusing. With advancing age, the lens becomes harder and stops changing shape, which results in the need for reading glasses. With time and further hardening the same lens becomes cloudy and eventually affects the ability to see, this is then called a cataract. Lens replacement is similar to cataract surgery in that the dysfunctional lens (and often clear lens) is removed and replaced with a sophisticated high performance intraocular lens implant measured specifically to suit each eye.
At Centre for Sight, a laser (rather than a manual technique) is used to assist the process in Lens Replacement / Exchange and is performed in this manner in 100% of cases and at no additional cost.
Suitability for Lens Replacement Surgery
Generally, those over the age of 50 with any level of hyperopia (farsighted), and 55 with any level of myopia (shortsighted) and/or astigmatism, can be suitable for Lens Replacement Surgery. Those who have cataracts are often suitable for high performance trifocal lenses, which provide a full range of focus.

Special Characteristics
The natural crystalline lens in the eye becomes harder with advancing age and in turn fails to change shape adequately to alter focus for near vision. A change in shape is necessary when looking at near objects e.g. reading a book or iPad.
The natural lens functions inadequately and the condition is termed by some as “Dysfunctional Lens Syndrome” (DLS). The crystalline lens becomes progressively harder and in turn near focus deteriorates further with advancing age. Reading glasses which become progressively stronger are needed to be able to see. This condition is also called Presbyopia. There are several options available to surgically correct Presbyopia using intraocular lenses and these are outlined below.
“Replacement of the poorly functioning natural lens with a high performance lens implant can result in complete spectacle independence!”
Different types of lens surgery?

This is the most common type of lens used for full vision correction at Centre for Sight (since 2011) with more than 90% of patients undergoing lens surgery with this type of lens implant. The advantage of this lens is it reliably provides correction of distance, intermediate and near vision, in other words a full depth of focus, eliminating or reducing the need for glasses.
Suitability for the lens implant is determined at consultation when numerous tests including the optical properties of the cornea and tear film are evaluated. To work well, these high performance lenses require a cornea with good optical properties as well as a surface free of dryness and no streaky tear film. Patients must understand the concept of adaptation or neuro-adaptation which involves the brain becoming accustomed to the new sophisticated optical system to pick up and interpret useful information. The lens has microscopic rings which provide near and intermediate vision and as a consequence patients may well experience transient halos that disappear with adaptation. Visual ability also improves with time from gradual neuro-adaptation.

For those who have already had lens replacement / exchange or cataract surgery and were not lucky enough to have a trifocal lens, there is an option of adding in a trifocal lens implant on top of the existing lens. This is also available at primary cataract surgery. For instance if someone has Glaucoma or macular degeneration, they may in time have a problem with the presence of a trifocal implant and may require removal. As an add-on lens placed on top of a monofocal, the lens can easily be removed from the eye. It is however reassuring that multifocal lenses have been in use at Centre for Sight since 2002 and to date no lenses have required removal for glaucoma or macular degeneration.
In those who have a significant amount of astigmatism, trifocal lenses with inbuilt astigmatism can be used to correct vision at all distances (Full range of Focus). These multifocal / trifocal lenses are specially ordered based on specific measures taken at consultation. In terms of performance, these are otherwise identical to Trifocal lenses discussed above. About 30% of patients at Centre for Sight require toric lenses.
See – Sheraz M. Daya & Marcela Espinosa-Lagana: Visual & Refractive Outcomes of a New Hydrophobic Trifocal Intraocular Lens
This type of lens referred by some as an EDOF (Extended Depth of Focus) lens is one that reliably provides distance and intermediate vision. To improve the range of focus further, the non-dominant eye is adjusted so that this becomes very slightly short-sighted, and this provides most patients with near vision. The lens is considered in those who are unsuitable for Trifocals (a full range of focus lens). The type of IROF lens used at Centre for Sight has some advantages in that there are no significant halos, however some like with the trifocals still require a period of adaptation to obtain optimum use of the lenses.
The single focus lens is used in conventional cataract surgery for instance in the NHS and vision is often geared for distance only which means recipients will in all probability require glasses for intermediate and near vision. Monovision is where the lens power can be adjusted to provide near vision in one eye (usually the non-dominant eye) and distance correction in the dominant eye. This provides good depth of focus between the two eyes and is very useful. For many the disparity between the two eyes is a nuisance and not everyone is able to get used to this option of Monovision sometimes also called Blended Vision.
This lens implant provides a greater range of focus than a standard monofocal implant. It is useful as an alternative in those not suitable for trifocals but wish to have increased range of focus. Distance and intermediate vision are often good however for near vision glasses are still required. A micro-monovision arrangement sometimes is used with one eye made very slightly myopic providing improved near vision with both eyes open.
Poorly termed, this lens like a Monofocal Plus increases the range of focus but with slightly better performance. The term EDOF comes from photography and Centre for Sight doctors are involved in devising new international terminology to address this confusion.
This article published in Cataract and Refractive Surgery Today- Europe “Let’s speak Lenspeak” authored by medical director Sheraz Daya provides some insight.

This is a lens that has astigmatism built in to the implant and used in those with astigmatism on their cornea of 1.25D and above. For those with less astigmatism, limbal relaxing incisions are at Centre for Sight performed using the laser employed in Lens replacement surgery. Toric lenses have to be specially ordered and sometimes need to be manufactured to suit the individual eye. This may increase the lead time for surgery. Toric lenses are available in combination with both Monofocal and Trifocal lenses.
The Consultation
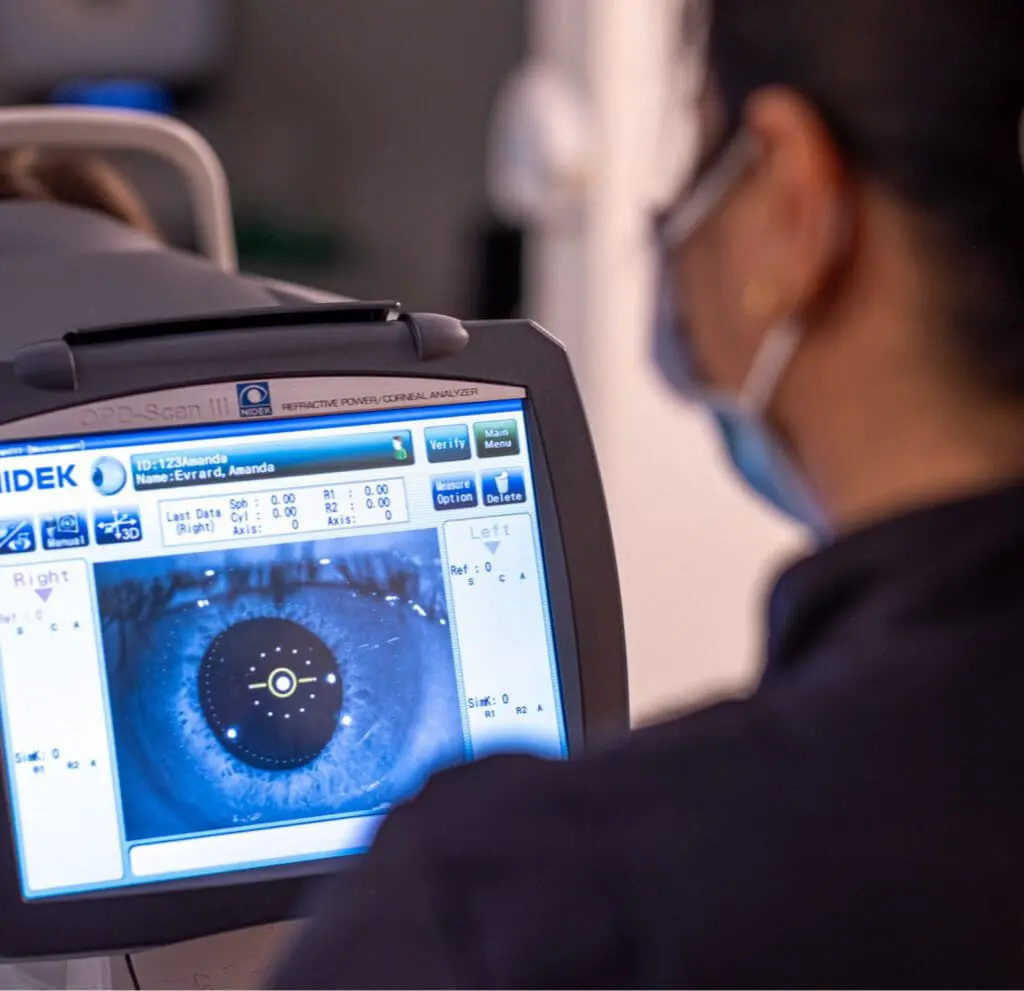
At Centre for Sight a thorough preoperative consultation will be conducted by the Consultant Surgeon who will carry out your procedure. The surgeon is supported by a team of highly trained technicians who perform a minimum set of investigations and measurements.
Based on initial findings, additional investigations may be required to further evaluate the eyes as necessary. During the process, ophthalmic technicians and optometrists are in constant contact with and directed by the Ophthalmic Consultant surgeon. Once this has been accomplished the patient will be seen and counselled further by the Consultant surgeon.


The Procedure
The procedure is typically performed under drop anaesthetic. At Centre for Sight most patients opt to have intravenous sedation which involves insertion of a venous cannula and periodic injection of sedatives to keep you well relaxed. Your pupils will be dilated with a series of eye drops and possibly with a medicine pellet under your lower lid. You will also receive strong antibiotic eye drops to kill bacteria and prevent infection.
Aftercare & Recovery
You will have some time to recover following surgery and when ready you will be served a light snack. You will be given a small toiletry bag containing your medications and instructions on their use. You will then be able to go home and we suggest you get plenty of rest that day.

Our Consultants





Author Information
Authored by Sheraz Daya MD FACP FACS FRCS(Ed) FRCOphth
Mr Daya is the Medical Director of Centre for Sight and listed amongst the 100 most influential ophthalmologists in the world (https://theophthalmologist.com/power-list/2018/sheraz-daya/).
Next review due January 2025.