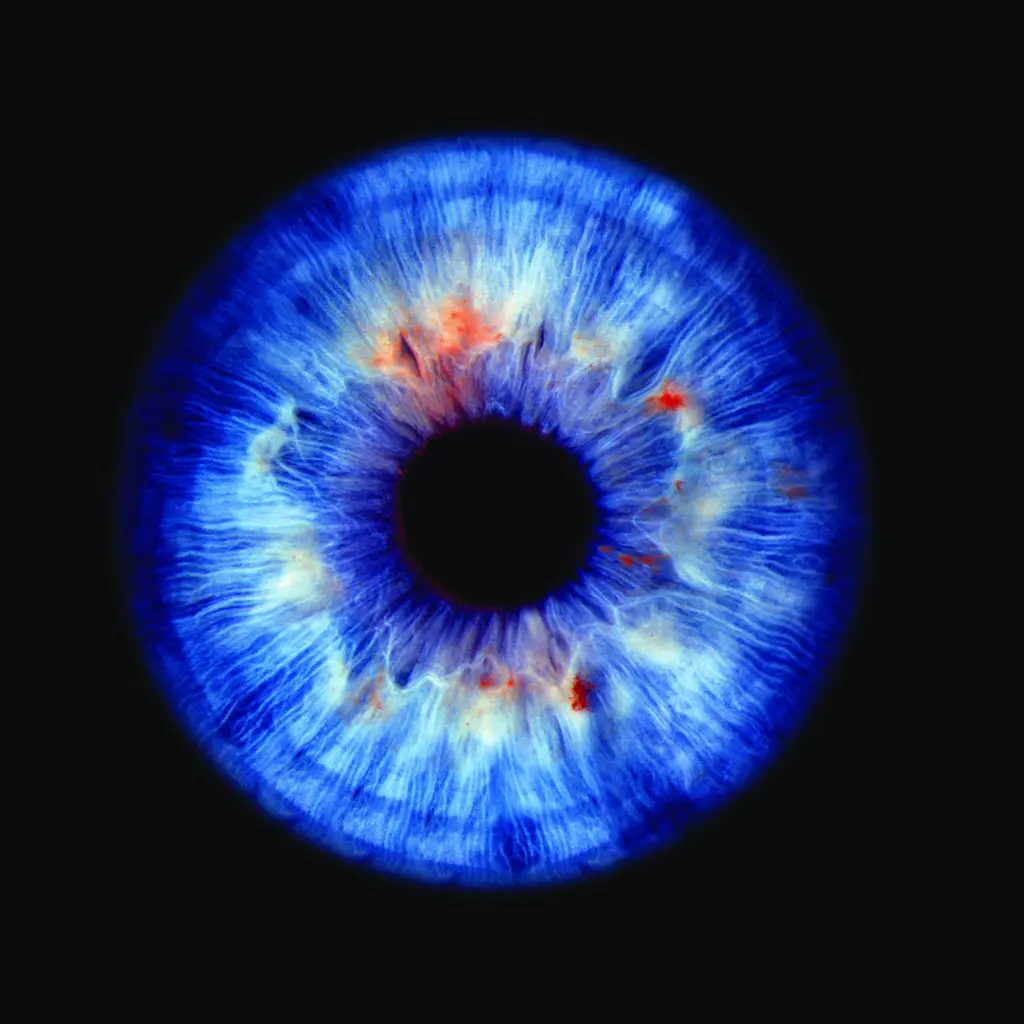
What is DSEK / DSAEK?
DSEK (Descemet’s Stripping Endothelial Keratoplasty) and DSAEK (Descemet’s Stripping Automated Endothelial Keratoplasty) are partial-thickness corneal transplant procedures used to treat diseases affecting the endothelial layer; the thin, innermost part of the cornea responsible for pumping out excess fluid and maintaining clarity.
When this layer fails (as in Fuchs Endothelial Dystrophy, pseudophakic bullous keratopathy, or post-surgical endothelial damage), the cornea becomes swollen and vision cloudy.
Unlike traditional full-thickness transplants, DSEK and DSAEK replace only the diseased inner layer, leaving the outer corneal structure intact. This results in faster recovery, reduced rejection risk, and more stable visual outcomes.