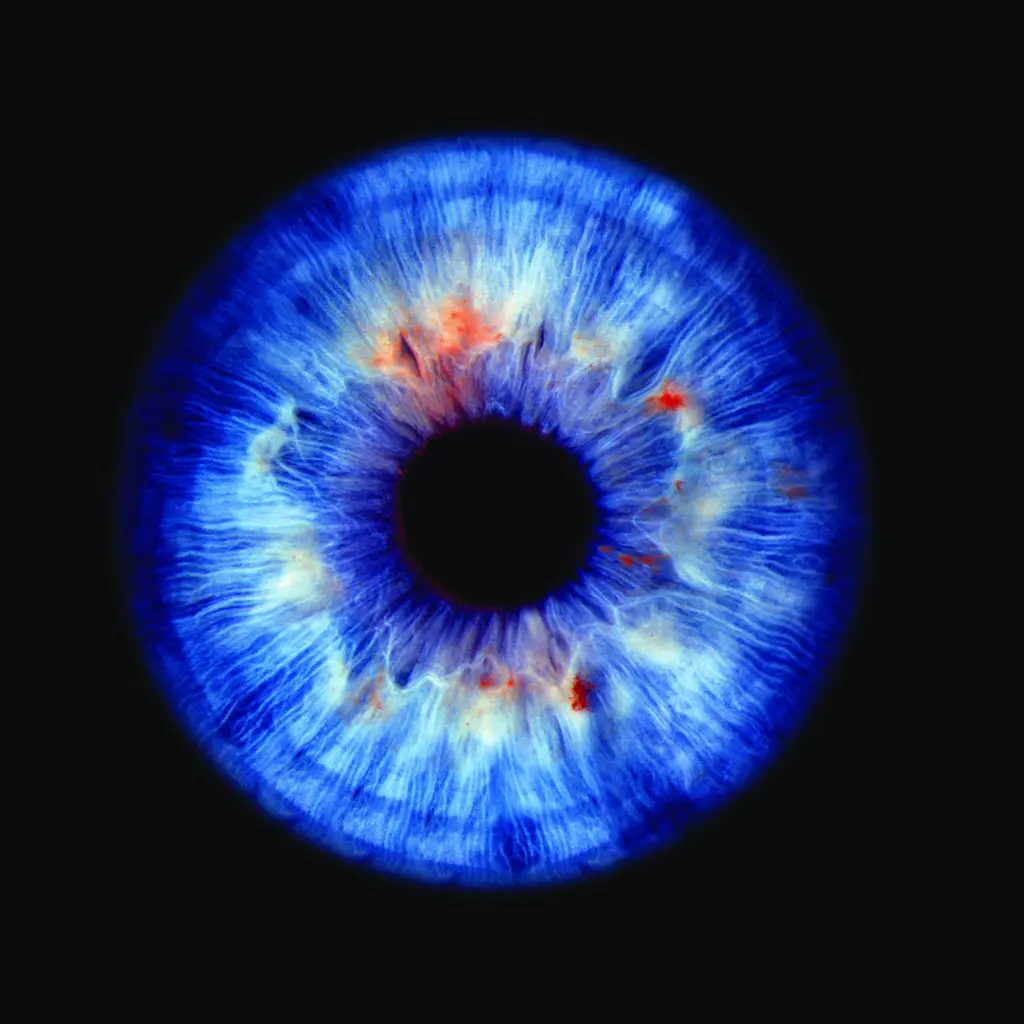
What is a Corneal Transplant for Keratoconus?
Keratoconus causes progressive thinning and bulging of the cornea into a cone shape, leading to visual distortion, increasing astigmatism and reduced contact lens tolerance.
When conventional treatments (glasses, rigid contact lenses, cross-linking) are no longer effective, a corneal transplant may be recommended.
A corneal transplant for keratoconus replaces all or part of the damaged cornea with healthy donor tissue, restoring shape, clarity and visual comfort. At Centre for Sight we often use Deep Anterior Lamellar Keratoplasty (DALK) or other graft techniques that preserve the patient’s own endothelium and reduce rejection risk.